Being on an Infertility Journey With Chronic Illness
Fertility Journey, Crohn's Disease and Motherhood
Amanda joins us to talk about her infertility story, how Crohn's Disease impacts that, and being a new mom dealing with chronic illness.
WHAT IS IT LIKE TRYING TO CONCEIVE WITH CHRONIC ILLNESS?
Hi, I’m Amanda! If you know me in person or follow me on social media ( @heartfeltbeginnings), you know a few things about my life, in no particular order. I openly share my infertility story and the journey to my daughter.
I have a 6-month-old daughter.
My partner and I struggled with infertility and went through IVF to conceive her.
Have a snuggly pup named Ollie (after Oliver Queen on the TV show Green Arrow).
I am a fierce advocate for mental health.
Have Depression and Anxiety and Crohn’s disease.
Believe in compassion.
I am an Enneagram 2.
My favorite book is is “If You Feel Too Much” by Jamie Tworkowski.
And most importantly, I find myself sitting with a lot of feelings and emotions on the regular.
Let me share more about the reason I’m here.
If there’s one thing I know for sure, it’s that I was born to be a mother. I started babysitting at age 11 and immediately was drawn to the art of caring for others. Also, I love children. I always have.
Our Dreams of Parenthood and the Entrance of Infertility Story
From the time my now husband and I started dating, we talk openly and extensively about our hopes and dreams with regards to our future and growing a family. Because I have Crohn’s disease, I did not exactly know what the journey to motherhood might look like for me. The more I was open about this, and the way it made me feel, the easier it was to talk to my partner about it. We talked specifically about how if I couldn’t get pregnant, or if I couldn’t stay pregnant due to my complicated health history, our hearts were open to both surrogacy and adoption.
After our engagement, our conversations began shifting from faraway dreams to close up action steps. With each passing day, my heart got louder and louder. I realized that I could not deny what I was feeling. I was adamant about trying any way possible in order to carry my first child.
The entrance of Maternal and Fetal Medicine in our Infertility Story
Being proactive (call it slightly neurotic, careful, worried, or just an experienced patient), we scheduled a meeting with a highly recommended Maternal and Fetal Medicine (MFM) physician. During our two hour appointment, we reviewed the most recent years of medical records, my prescription history, and my current medications and supplements. The MFM suggested a couple of small changes, and then we were sent on our way with “official” approval to start trying to conceive. We were ecstatic and so grateful. Truthfully, as a Crohn’s patient, it’s rare that I walk out of any doctor’s appointment feeling optimistic. This felt like a sign that my body might let us move in the right direction.
READY TO INTENTIONALLY TRY TO GET PREGNANT
I went out and bought two different ovulation testing kits, and found an app for my phone to keep track of everything. Along with that, I even made my husband download it so he could see in advance what days would be most important for being intimate.
@amanda.osowski
This was all well and good, except 8 months passed without any success. My Crohn’s disease was managed better than it had ever been, and yet, I still wasn’t pregnant. Every time my period came, my heart sunk a little more. I became concerned that maybe Crohn’s disease was standing in my way of conceiving. I also noticed some inconsistencies in the length of my cycles, so I scheduled an OB/GYN appointment with my regular doctor. Then, she recommended that my husband go for a semen analysis, and said that she would follow up with us after she got the results.
Infertility Story: It's Not Just From Crohn's Disease
Her insight that Crohn’s alone shouldn’t be preventing us from getting pregnant was correct. My husband’s analysis was deemed “poor” - indicating a lower number of sperm, reduced sperm motility and abnormal sperm shape/size. It was then that my OB/GYN let us know that we would not likely be able to get pregnant without the help of technology.
I feel horrible to admit that this provided me a sense of relief. My husband is as healthy as a horse. Besides a running injury and kidney stones, he has only seen a doctor for a few colds or sinus infections in the 5.5 years I have known him. To hear outright that my non-chronically ill spouse was also experiencing problems impacting fertility helped me realize that our challenges in conceiving may not be because I have Crohn’s.
The Transition to Infertility Specialists
After nearly a year of trying to conceive naturally, our fertility journey transitioned from something we talked about only inside the walls of our apartment to something we spoke about often, and in public. Next, with the help of a Reproductive Endocrinologist and Infertility Specialist (REI), my husband and I both went through a series of tests, hopeful we would obtain a diagnosis or a reason for our infertility story.
Unexplained Infertility
The positive was that his analysis results improved, and all of my tests came back completely normal. The negative was that this meant our challenges with conceiving fell under “unexplained infertility.” This new diagnosis felt cold and hard and frustrating. Much like my Crohn’s disease, there wasn’t one specific thing that caused our struggles with our infertility story, and there wasn’t one certain route to fixing them either. Emotionally, I was transported to the years before my Crohn’s disease diagnosis. I felt vulnerable, frustrated, and discouraged.
INTRAUTERINE INSEMINATION (IUI)
Our REI recommended we start with Intrauterine Insemination (IUI), and if we were still not pregnant after at least three successive cycles, we would move on to In-Vitro Fertilization (IVF). Although the intended outcomes differed (better health vs. carrying a child), the feelings were so similar to me. Both IBD and infertility were filled with the same set of emotions: Hope. Fear. Heartache. Cautious Optimism. Patience. Preparedness.
Compared to the medical tests, procedures, and treatments I have experienced in relation to my Crohn’s disease, the IUI experience was gentle and uneventful, and the actual procedure itself was fairly anticlimactic.
The Waiting Between Treatments
To be honest, the hardest part of the process for me was what came next. After the procedure, you cannot take a pregnancy test for two weeks. The waiting was incredibly anxiety-provoking. It felt like every time I had waited for the pathology reports from a scope, or the results from labs or the doctor to call me back. I couldn’t do anything but be patient.
Our first IUI was not successful. When my period arrived, I felt such deep and significant heartache. We had done everything right, and yet, we were still unlucky. What I realized though was that I had been in this place before. This place always only had to do with me and my health, and not my husband or the child we were trying to create, but it was still a familiar place.Devastation.Disappointment.Frustration.Fear.I had already cultivated coping mechanisms during trials and tribulations with my Crohn’s disease, and I felt relieved knowing I didn’t have to pave an entirely new path in these moments.
Two Failed IUIs
Our second IUI also failed. As a somewhat professional patient by this point in my life, I reflected on the idea that completing the third cycle in exactly the same way felt repetitive and was unlikely to succeed. Based on my history, our REI (Reproductive Endocrinologist and Infertility Specialist) instituted an autoimmune protocol, adding a low dose of prednisone during the first half of my cycle, and a combination of antihistamines from the day of the IUI through test day. We did not get lucky with our third or fourth IUI either.
Let me tell you that the waiting period - it does not get any easier with time or repetition. And the disappointment, while no longer a surprise, still burned.
My husband and I then moved forward with IVF.
IN VITRO FERTILIZATION
The IVF process was more time-consuming, more invasive, and more emotional than the IUI’s we walked through, but knowing the chances of success were higher we marched forward as best as we could. Twice-daily injections, daily monitoring visits (including bloodwork and a transvaginal ultrasound) and the high dose of hormones affected me so much, but the dream of being a mother gave me the courage to continue on.
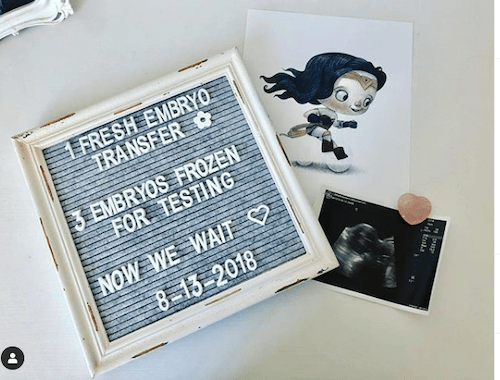
After 13 days of stimulating my ovaries, I had my egg retrieval procedure, where they removed 12 eggs, of which 8 fertilized, and 4 matured into embryos. 5 days later, I went through a fresh embryo transfer. The 8 days that followed between the procedure and being able to test for pregnancy were torture, and the negative tests that followed really affected my husband and I. We were so disappointed.
Embryo Genetic Testing
At that point, we chose to have the 3 embryos we froze genetically tested to ensure they were chromosomally normal before they were transferred back to my uterus. This made me feel a lot more confident about our second cycle, which ended in a successful frozen embryo transfer.
I took a positive pregnancy test at the end of September 2018, and outside of “normal” pregnancy challenges: morning sickness, exhaustion, aches and pains, heartburn, and frequent urination, my health, and my IBD remained relatively consistent during my pregnancy. This can be attributed this to two things: I continued the exact treatment plan I was on when I found stability and entered remission, AND, I was incredibly lucky.
WHAT DID YOU KNOW ABOUT POSTPARTUM PRIOR TO YOUR OWN INFERTILITY STORY?
This answer will, unfortunately, be much shorter! I didn’t know very much at all about the postpartum experience. My labor and delivery doula had encouraged me to get some pads before I had the baby, and some nursing bras, but that was probably the extent of my preparation/knowledge.
WHAT SURPRISED YOU ABOUT YOUR POSTPARTUM EXPERIENCE?
I didn’t know I was going to bleed for what felt like forever! (Okay, 4 weeks, but still) I had NO idea about pumping, hands-free pumping bras, or exclusive pumping, and that was learning and trial by fire. Also, I didn’t know that my hormones would fluctuate and change for so long after delivery – I thought by the time the fourth trimester ended I would be back to “normal.”
HOW DID OTHERS RESPOND TO YOUR POSTPARTUM EXPERIENCE? - WORKPLACE, CLOSE FRIENDS AND FAMILY, STRANGERS?
Honestly, I controlled a lot of the narrative, which I’m really grateful for (mostly because I chose to share both the great and the hard). I had been laid off from my job during my pregnancy. I wasn’t working when I gave birth and I didn’t start looking for a new job until a few months postpartum. There was no workplace/colleague response for me. My close friends that are moms did a lot of “me too” and “yes girl” encouragement to things I shared. Thankfully, they were available for questions/conversation, but to be honest I felt surprised (and a little sting) that they hadn’t shared more/warned me during my pregnancy of what was to come.
WHAT DO YOU WISH MORE PEOPLE REALIZED ABOUT POSTPARTUM AFTER INFERTILITY AND IN THE MIDST OF ONGOING ILLNESS?
For me, my postpartum experience has been much harder as a chronic illness patient. Not only have I had to manage my postpartum body, physical mental, and emotional changes, and my baby, and the whole breastfeeding/pumping situation. I had to watch my Crohn’s disease like a hawk. Making time for infusions and medication, and doctors appointments and routine labs, and to maintain vigilance too in case my symptoms started flaring.
I wish people realized how hard it was for me to manage everything. Think about everything. Have to feel in control of so much. To still be expected to entertain visitors and write thank you notes. I wish people realize that sleep is critical for my Crohn’s disease. And while the new parent badge of honor is running on fumes, that was actually a danger to my health. etc.
RELATED: The Postpartum Cookbook
WHAT ARE SOME OF THE THINGS THAT PEOPLE SAID/DID THAT WERE HURTFUL RE: ILLNESS OR FERTILITY?(EVEN IF WELL-INTENTIONED?)
I didn’t know about it until I began walking through it, but like IBD, conversations about fertility come with an associated stigma.
As many IBD patients have probably experienced at one point or another, being open about the intimate details of Crohn’s disease with family and friends is challenging. I remember when I first became symptomatic, I tried to remain as vague as possible.
Private Life in Secret
Even though it was one of my main frustrations, I completely avoided the word diarrhea. I used to feel like it was too embarrassing to say out loud! Without being comfortable talking about how I was feeling, I became a much quieter, more introverted person during the first few years I was sick. I t felt like my private life had to hold all of my secrets, and it became easier to put less and less out into the world.
How Little Fertility/Infertility is Discussed
In the time my husband and I tried to conceive, we realized how little fertility is discussed. Everyone celebrates pregnancy announcements and births. But in many circles, things like timed intercourse and tracking ovulation are not talked about. However, in my experience, when we were unable to conceive naturally, this divide in conversation became increasingly pronounced. Within a few months of our wedding, family and friends started asking when we were going to grow our family.
Amanda's Infertility Story Quotes
I found myself saying open-ended and non-specific things like “we want to” or “it’s something we are hoping for.”It felt completely off-limits to tell them that we were trying everything we could to conceive.
I started to wonder why I was prohibiting myself from being honest, and I realized that I felt ashamed about failing to get pregnant on my own.
Feeling At Fault
Similar to when I first began struggling with IBD, I felt like maybe our challenges with infertility could somehow be my fault. Although this is of course not the case for either situation, I realized I was feeling parallel emotions - embarrassment, frustration, fear. By not talking to my friends and family, I was re-creating the conditions that led me to fold up around myself years ago.
WHAT ARE THE THINGS PEOPLE SAID/DID THAT WAS MOST HELPFUL IN A DIFFICULT TIME OF YOUR INFERTILITY STORY?
People who asked“What do you need?” instead of “Ask if you need help” opened the door with more concrete and honest feeling invitations to jump in with support. Also, more than the average bear, I wanted emotional support both during illness/infertility and postpartum.
RELATED: How to Start Exclusively Pumping (Online Course)
Postpartum Narratives
This series, Postpartum Narratives, brings awareness, normalization, and understanding to different postpartum experiences. No two postpartum experiences are the same. As a society, we cannot have one view of what postpartum is or should be. By sharing stories, we diversify our own understanding and can then advocate for better support and resources for each person and space that affects a postpartum family- the home, the workplace, the medical field, social constructs, etc.If you have a postpartum narrative you would like considered for contribution, please contact me here.
We provide free content as a priority at Postpartum Together. This page may contain affiliate links. This means, at no additional cost to you, we may receive a commission for your purchase. Don’t worry, we only promote things we believe in because we love you!